CRIS has been an integral part of our research into the COVID-19 pandemic.
The COVID-19 pandemic had wide and unforeseen consequences across health sectors. These included profound effects on mental health and mental health services. CRIS played an important role in helping us understand these effects and improve care.
When the lockdown began the CRIS team worked to turn around research activity and focus on the pandemic and its consequences for people using mental health services.
As well as setting up a number of studies, the team prioritised a series of initiatives to improve the usefulness of CRIS data. These included seeking permission for regular updates from the Acute Trust partners on emergency or hospital care by South London and Maudsley NHS Foundation Trust service users over the pandemic period, as well as making good use of the CRIS data linkage already set up with local GP records.
Read Professor Robert Stewart's blog on CRIS in the time of coronavirus to see more about how CRIS was used.
Pre-print publications
Preprints publications are research papers that have not been peer-reviewed or accepted by traditional academic journals. The benefits of pre-prints are that study information and data can be made publically available in a shorter timeframe however findings and conclusions have not been reviewed by other independent scientists as they would in a post-print published journal paper.
Pre-print publications
27 October 2020
Authors: Professor Robert Stewart, Amelia Jewell, Matthew Broadbent, Ioannis Bakolis, Jayati Das-Munshi
The CRIS team have analysed the recorded underlying causes of death in SLaM service users for March-June in 2020, coinciding with the peak of the first COVID-19 wave in London, comparing data to causes from the same four-month periods in 2015-2019.
There were 2561 deaths in March-June 2020, an excess of 1109 compared to previous years. There were a total of 708 deaths in 2020 with COVID-19 as the identified underlying cause, accounting for 63.8% of this excess. The remaining excess deaths were in the unnatural/unexplained category and caused by a mental/neurological disorder, with other causes showing no consistent excess.
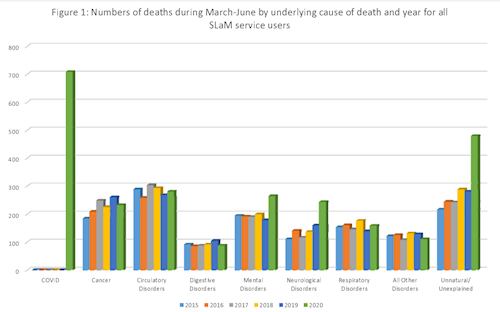 For other analysed categories:
For other analysed categories:
- 2% of deaths due to COVID-19 occurred in those aged 70+ years and over 80% occurred in previous rather than current service users.
- There was a male excess in deaths due to COVID-19 and in unnatural/unexplained deaths while excess deaths due to mental/neurological conditions were more marked in females.
- Data showed a higher proportion of COVID-19 deaths in patients of Black African/Caribbean ethnicity (37% of deaths, compared to 26% in White British and 27% in those from other ethnic groups)
- Data also showed a higher proportion of unnatural/unexplained deaths in those from other ethnic groups (24%, compared to 17% in White British and 16% in Black African/Caribbean patients).
Professor Rob Stewart said:
“We think that this information from SLaM may be unique for England for some time to come, because we don’t believe there are any other Mental Health Trusts with this data currently available.
As well as the COVID-19 related deaths which accounted for 64% of the overall excess in 2020, there are clearly concerns around the higher deaths attributed to dementia and the large number of unexplained deaths currently awaiting coroner inquests, which will include those due to suicide. No excess was seen in deaths due to physical illnesses like cardiovascular disease or cancer, but we’re only looking at the four months around the first wave of the pandemic here, and we don’t know what the longer-term consequences will be.”
Mental health service activity and mortality during COVID-19 lockdown among individuals with: neurodevelopmental disorders and personality disorders
13 October and 14 September 2020
Authors: Evangelia Martin, Eleanor Nuzum, Matthew Broadbent and Professor Robert Stewart
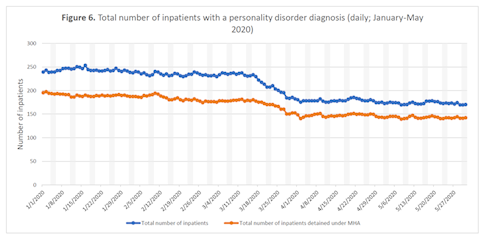
Lockdown and social distancing due to COVID-19 are likely to have had widespread impacts on mental healthcare service provision and use. In these two studies, our researchers quantify activity for individuals with neurodevelopmental disorders and personality disorders.
Comparing periods before and after the 16th March 2020:
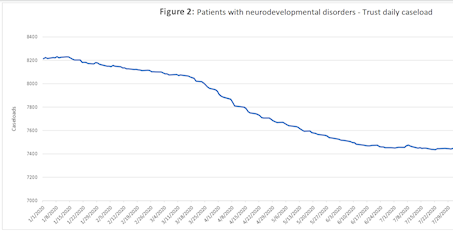
- For neurodevelopmental disorders (January to July 2020): Mean number of accepted referrals decreased by 32% and caseloads were reduced in all specific services. Overall, total caseload numbers remained relatively unchanged with a 6% decrease, although inpatient numbers were reduced more substantially by 22% because of discharges made in the early period of lockdown.
- For personality disorders (January to May 2020): Daily caseloads showed reductions across services while mean daily deaths increased by 28%. There was a large 36% decrease in the number of accepted referrals and a small 4% decrease in the number of discharged patients and in total caseload. A marked decrease in inpatient admissions of 43% was seen while a smaller decrease in inpatient discharges (by 14%) accompanied a decrease by 23% in the total number of inpatients for diagnostic group.
- Daily numbers of deaths had increased in both groups during the March to May period: by 28% in people with personality disorders, and by over 280% in people with neurodevelopmental disorders. In common with reports for other service user groups, contacts with many services had moved substantially from face-to-face to virtual arrangements.
 Professor Robert Stewart says: "We wanted to describe the experiences of both of these groups because they are often a little lost in general mental healthcare statistics.
Professor Robert Stewart says: "We wanted to describe the experiences of both of these groups because they are often a little lost in general mental healthcare statistics.
Both groups clearly experienced substantial changes in their contacts with mental healthcare over what was a challenging period.
The higher mortality rates are clearly very concerning and need further attention, particularly as we enter a second wave of the pandemic."
28 September 2020
Authors: Professor , , , , ,
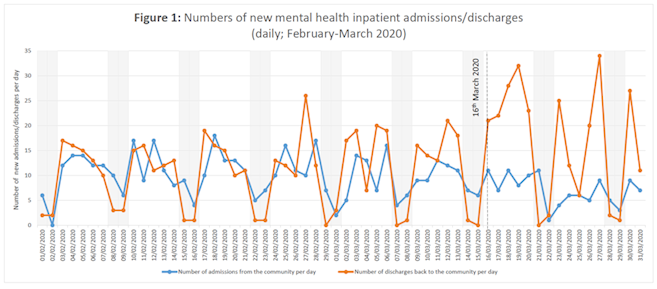
This study describes early changes in mental health service activity before and after social distancing for COVID-19 was implemented, by comparing activity before and after 16 March 2020 up to the end of March for:
- inpatient admissions, discharges and numbers
- contact numbers and daily caseloads (Liaison, Home Treatment Teams, Community Mental Health Teams
- Numbers of deaths for past and present patients.
Daily caseloads fell for all services, apart from working age and child/adolescent community teams. All grouped liaison, home treatment and community mental health services had substantially reduced face-to-face patient contacts, with variable and only partial compensatory increases in non-face-to-face contacts.
Inpatient numbers fell 13.6% after 16th March, and daily numbers of deaths increased by 61.8% during that period.
Professor Robert Stewart says:
"We are putting this information in the public domain, as it describes a very early point in the first wave of the pandemic which presented substantial challenges to mental healthcare. We were pleased to be able to turn around the manuscript very rapidly at the time, although had less satisfactory experiences with conventional publication routes which have been influential in the alternative means of dissemination being trialled on this site."
14 July 2020
Authors: Professor Robert Stewart, Matthew Broadbent and Jayati Das-Munshi
The COVID-19 pandemic has been accompanied by excess all-cause mortality at a national level. CRIS researchers previously described a 2.4-fold excess mortality in past and present SLaM service users during the period of the pandemic from 16 March to 15 May 2020 to that for the same period in 2019. In this pre-print our researchers compared mortality within specific ethnic groups.
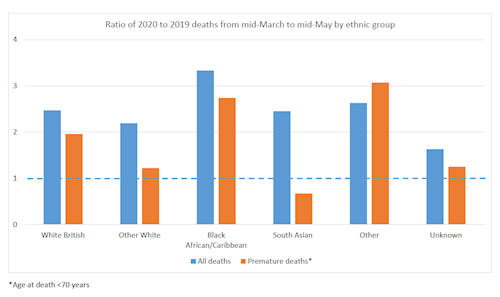 When examined by recorded ethnicity, the ratio of total deaths between the two years was highest at 3.33 in Black African/Caribbean patients and those from other ethnic groups at 2.63, compared to 2.47 in White British patients.
When examined by recorded ethnicity, the ratio of total deaths between the two years was highest at 3.33 in Black African/Caribbean patients and those from other ethnic groups at 2.63, compared to 2.47 in White British patients.
Considering premature deaths (age at death below 70), 2020:2019 ratios were 3.07 for other ethnic groups and 2.74 for Black African/Caribbean patients compared to 1.96 for White British patients.
Professor Robert Stewart says
"Unfortunately these figures speak for themselves and show the sizeable inequalities in mortality that have been described at a national level. I could say that the results are unsurprising, but then perhaps the problem is that we’ve stopped feeling surprised. Clearly this is as much a challenge for SLaM as for everywhere else."
 Using past and current data to estimate potential crisis service use in mental healthcare after the COVID-19 lockdown: South London and Maudsley NHS Trust data
Using past and current data to estimate potential crisis service use in mental healthcare after the COVID-19 lockdown: South London and Maudsley NHS Trust data
30 June 2020
Authors: Professor
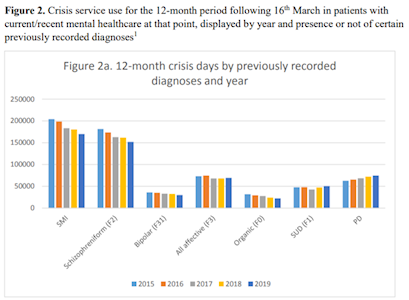
The CRIS team have estimated service use by those most likely to receive crisis care in the 12 months following UK COVID-19 policy on 16 March 2020.
Comparing data from 16 March 2015-19 the CRIS team found that over 80% of crisis days at SLaM were accounted for by inpatient care, 75% were used by patients who were current or recent Trust patients at the start of follow-up, and highest numbers were used by patients with a previously recorded schizophreniform disorder diagnosis.
For current/recent patients on 16 March there had been substantial reductions in use of inpatient care in the following 31 days in 2020 but no significant change in total non-inpatient contact numbers.
Professor Robert Stewart says:
"The wealth of information in the health record is allowing us to learn from previous years what we might expect in the year ahead. Taking advantage on the 24-hour updates from CRIS, we are putting in place monitoring processes to warn us early if demand on particular services moves beyond that previous experienced."
16 June 2020
Authors: Professor ,
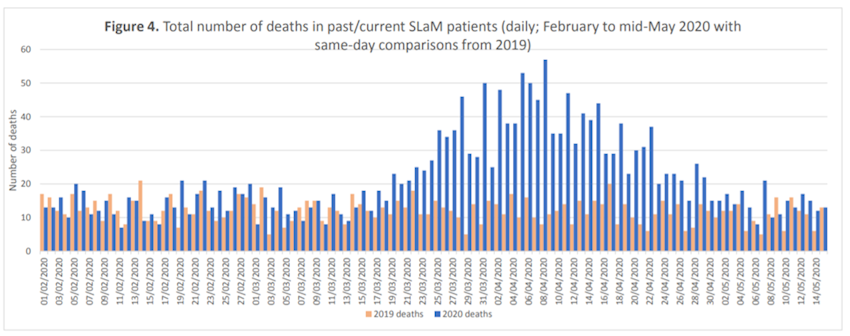
This paper describes daily caseloads and contact numbers (face-to-face and virtual) for home treatment teams (HTTs) and working age adult community mental health teams (CMHTs) from 1 February to 15 May 2020 at SLaM.
The CMHTs sector showed relatively stable caseloads and total contact numbers, but a substantial shift from face-to-face to virtual contacts, while HTTs showed the same changeover but reductions in caseloads and total contacts (although potentially an activity rise again during May).
The number of deaths for the two months between 16 March and 15 May were 2.4-fold higher in 2020 than 2019, with 958 excess deaths.
Professor Robert Stewart says:
“While it is reassuring to see that the mortality in SLaM service users has fallen back to 2019 levels, the number of deaths from March to May are still clearly concerning.
We believe that the excess mortality is higher than would be expected in the general population, reflecting the vulnerability of mental healthcare service users to this and potential future outbreaks."