Using neuroimaging to target treatment in psychosis
Approximately 30 per cent of people with schizophrenia and other psychotic disorders such as bipolar disorder, do not experience a beneficial response to standard antipsychotic medications.
These individuals have poor clinical outcomes, find it harder to manage their day-to-day lives and have much higher ongoing healthcare costs. There can be significant delays of many years (typically 4-6 years) in identifying these patients before initiating alternative treatments, like clozapine, the treatment typically prescribed for individuals resistant to conventional antipsychotics.
Chemical messenger indicates positive response to medication
Imaging research worldwide, including some conducted at the National Institute for Health and Care Research (NIHR) Maudsley Biomedical Research Centre, have consistently shown that dopamine, a chemical messenger, is increased in a brain region called the striatum in people with psychotic disorders, as well as people at high risk for psychosis. Differences in dopamine functioning can also indicate a variation in treatment response. For example, the capacity of brain cells to produce dopamine is elevated in patients who respond well to standard antipsychotic medications but unaltered in non-responders. This is called dopamine synthesis capacity
This dopamine synthesis capacity can be measured using positron emission tomography (PET) scanners using a radioactive tracer called [18F]FDOPA. This tracer is introduced in tiny quantities into a person’s blood stream and is attracted to regions in the brain that produce dopamine and because of its radioactive characteristics, it can be visualised using PET scanning. This technique could support clinicians in identifying patients who may require alternative treatment early on.
Simple PET scan can predict treatment response
We recently revisited our database of ~100 [18F]FDOPA PET images of patients diagnosed with psychosis, and we have strong evidence that a brief, simplified PET scan, adapted for clinical practice, produces a similar ability to predict treatment response. Our preliminary results show that we can identify between 40-50 per cent of individuals who would not benefit from a standard antipsychotic drug. This method is also specific and does not misclassify those who would benefit from standard antipsychotics.
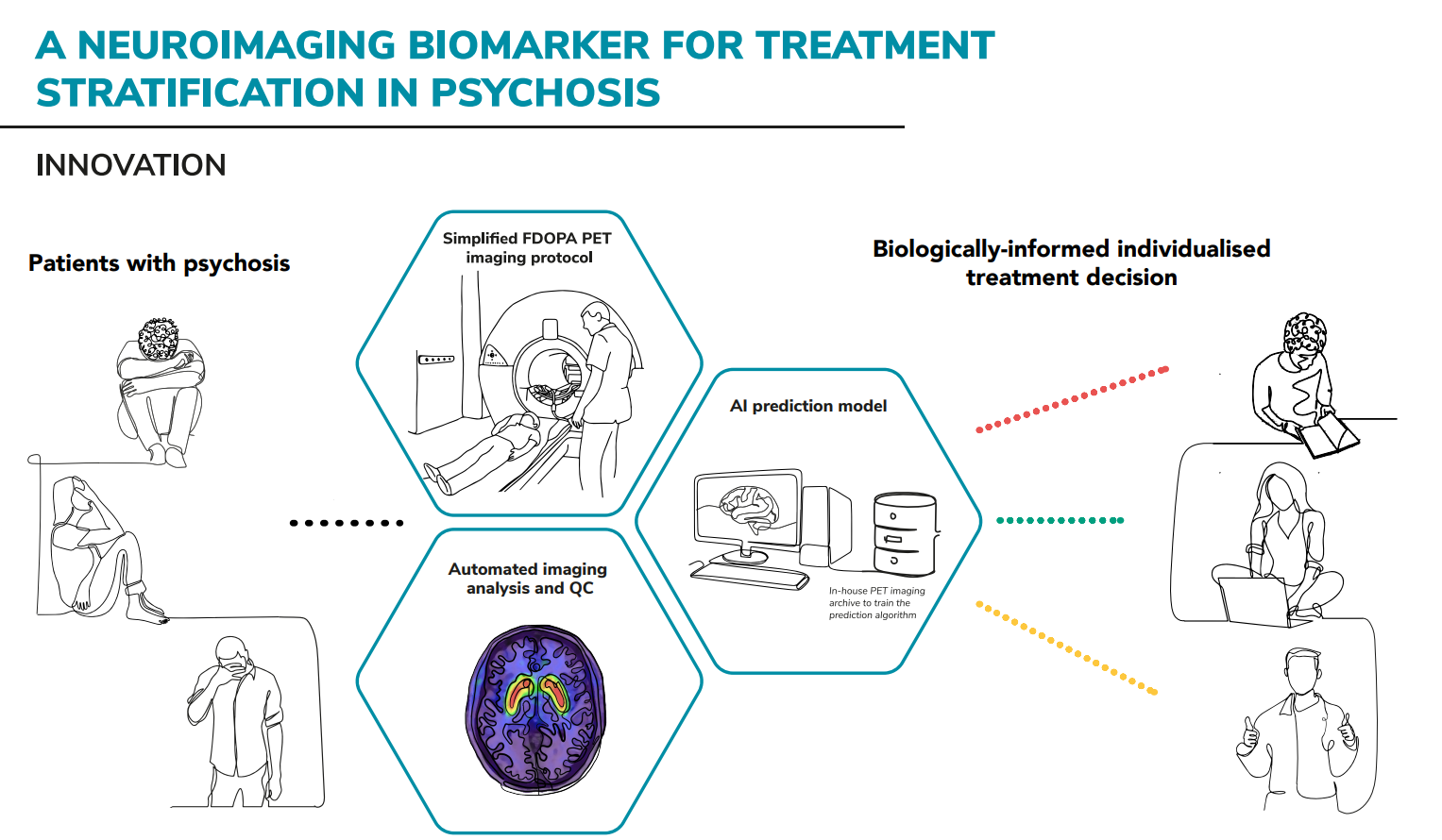
This technique has the potential to transform the care of people with psychosis by preventing those unlikely to respond to standard antipsychotics from being exposed to unhelpful medicines, and by improving their chances of earlier recovery with a different medication. We estimate that the economical and health care benefits are much higher than the cost for its implementation (approximately £3400 saved per patient).
IMPACT AREAS: