Digital therapy to treat distress in long-term physical health conditions
In the UK, at least 15 million people have a Long-Term Health Condition (LTC) and 30 per cent experience anxiety and/or depression.
Long-term health condition patients typically receive unconnected treatment from physical and mental health services or no psychological support. Co-morbid mental health disorders in long-term health conditions result in poorer clinical outcomes from existing therapies and a 45 per cent increase in healthcare costs.
Treating mental and physical health together
COMPASS provides online psychological treatment for people experiencing related anxiety and depression (distress) related to long term health conditions. Patients access support when convenient to them with minimal remote support from a therapist.
Unlike other digital cognitive behavioural therapies for anxiety and depression, COMPASS has the long-term health condition at the heart of the programme, and treats mental and physical health together. Eleven online modules address these-specific psychological challenges for long-term health conditions such as managing illness related uncertainty and coping with symptoms.
COMPASS is based on a model developed by the team, underpinned by research evidence on specific psychological and social mechanisms contributing to distress in long-term health conditions. These processes are targeted using pre-programmed, tailored interactive techniques. Extensive stakeholder engagement (patients, healthcare professionals) continues to inform improvements for usability and acceptability.
Patient Testimonial: Penny's Story
Implementation of COMPASS
COMPASS is CE marked. King’s Health Partners’ (KHP) Mind & Body programme supported development and implementation over four years, whilst King’s College London Commercialisation Institute helped develop a commercialisation strategy.
COMPASS has been implemented in Improving Access to Psychological Therapies (IAPT) service and KHP acute services. Findings show that patients’ depression, anxiety and daily functioning significantly improved (Figure 1, below). Patients liked the tailored content, online flexibility, and therapist support. There are on-going talks with other IAPT services interested in implementing COMPASS, having also launched in the Hackney IAPT service in January 2022.
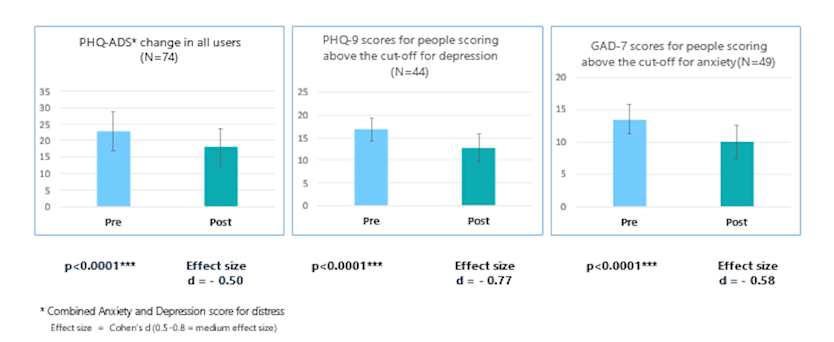
Figure 1. Real world data from NHS implementation feasibility study.
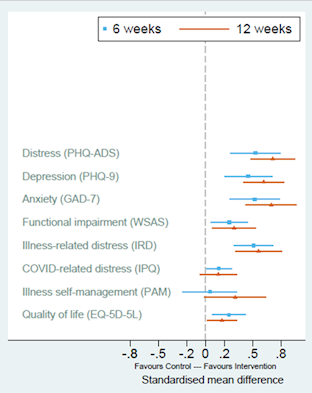
Figure 2: Treatment effects for COMPASS versus control (Standard Charity Support) on primary (PHQ_ADS) and secondary outcomes.
A randomised controlled trial evaluated COMPASS, working with five national long-term health conditions charities. Compared to standard support, COMPASS improved symptoms of depression and anxiety whilst also improving a person's ability to function and self-manage their illness (Figure 2).
The current version of COMPASS is applicable across all long-term physical health conditions. We plan to create illness-specific adaptations, such as diabetes, as well as a self-guided version to increase reach beyond primary mental health services, which only 4 per cent of the target population access (May 2021). Avenues include prescription via GPs, insurers and direct-to-consumer. International markets include USA and Germany, and future adaptations will include foreign language capabilities.
IMPACT AREAS:
Whole Person Care | Involving Patients in Research | Novel Diagnostics and Therapeutics | Improving Access and Uptake